Umming and ahhing about whether to get an IUD? The introduction of emergency pain relief for outpatients by one Melbourne Hospital could be a game changer.
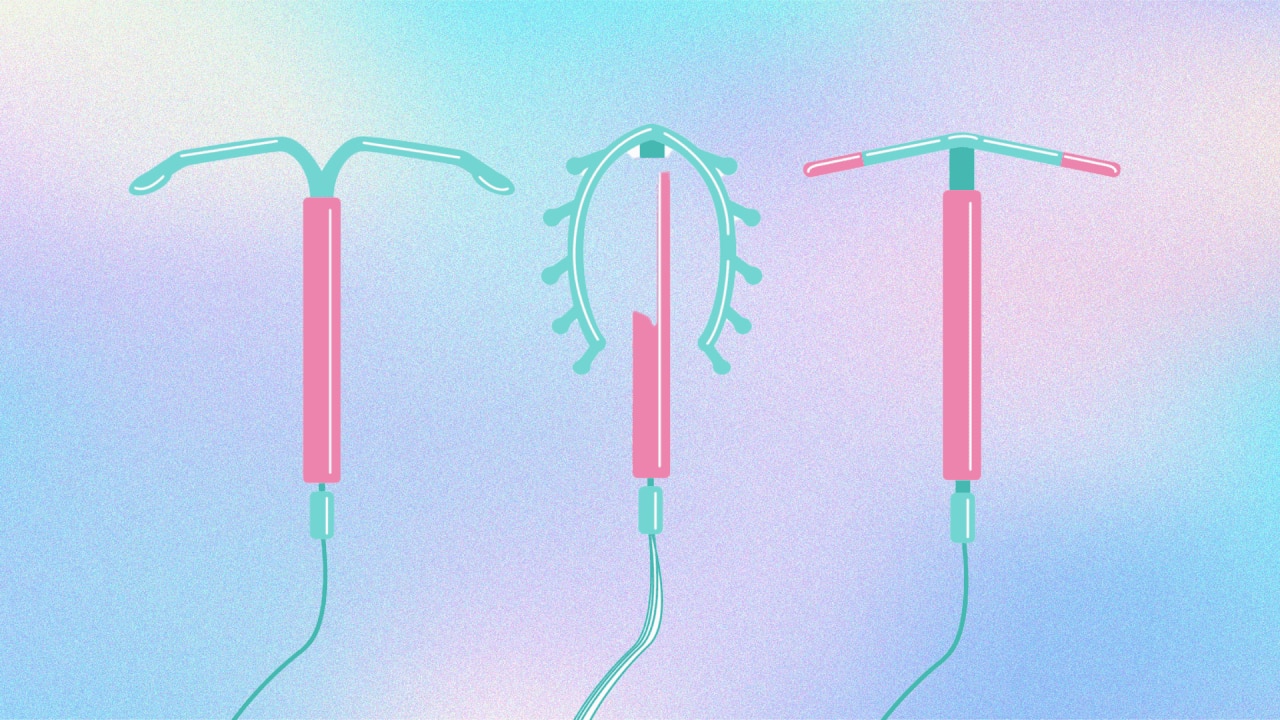
Of all the forms of contraception on offer to women, IUDs, particularly the hormonal kind (also known as the Mirena) have emerged as one of the favourites.
Lasting up to eight years, the Mirena is reportedly over 99 per cent effective at preventing pregnancy – thanks to the lack of human error – and the best part is, it’s a totally reversible form of contraception.
But for all their pros, for anyone looking into getting an IUD, there’s one part of the process that can be a bit of a turnoff: getting it inserted into your uterus, without pain medication, while you’re awake.
As such, IUD rates in Australia are low as compared with the rest of the world. But now, one hospital in Melbourne has decided enough is enough.
Like what you see? Sign up to our bodyandsoul.com.au newsletter for more stories like this.
Frankston Hospital, a public hospital near Mornington, Victoria, has become one of the first in Australia to offer outpatients the ‘green whistle’ when undergoing IUD insertion.
Most commonly seen on Bondi Rescue and the sidelines of sports games, the green whistle is an emergency form of pain relief. The drug itself is an analgesic called Penthrox, which is administered via breathing in through a tube with a recorder-esque mouthpiece.
Per the ABC, Frankston Hospital started trialling use of Penthrox for IUD procedures “a few months ago”, and is now offering the pain relief to everyone undergoing IUD insertion or removal.
Some GPs and sexual health clinics already offered the pain relief to their patients, but Frankston is one of the first hospitals to do the same – a great advance in terms of accessibility, particularly in the public system.
Dr Nisha Khot, head of obstetrics and gynaecology at Peninsula Health, said thus far, use of the green whistle has been “popular” amongst IUD patients.
„There are some women, especially younger women, or women who previously had a bad experience with an IUD insertion, who really are very reluctant to have it done in that sort of outpatient setting.
„And we’ve said to these women, look, here’s something that you could use, see how it works for you.“
Dr Nicole Higgins, president of the Royal Australian College of GP, said that this level of wariness has likely come about from word-of-mouth reviews: “Unfortunately, one person’s bad experience will colour many others, „she said.
„We don’t tend to talk about the good experiences; only the difficult ones.“
Anecdotally, many women have experienced severe pain having their IUDs inserted by GPs in an outpatient setting, describing it as one of the worst kinds of pain they’ve ever experienced.
For those unwilling to go through it, you can have the IUD inserted while under general anaesthetic – but the process is more lengthy and there are risks associated with going under general. Not to mention the extended wait time that would be tacked on to have the more comprehensive out-patient procedure in the public system, time many people cannot afford.
The Mirena was invented in 1990, meaning women have been undergoing a potentially very painful procedure without available pain management for over 30 years. It’s not a new phenomenon, women’s pain and conditions that affect women have been disproportionately sidelined for hundreds of years – or in some circumstances, barely researched at all.
Thus it’s great to see IUD insertion at the forefront of the news cycle, with meaningful adjustments being implemented to make contraception more accessible for many – an undeniably positive step forward for women’s health and sexual freedom.
Let’s hope other hospitals and private practitioners are soon to follow suit.